
The 97530 CPT code plays a critical role in medical billing for therapists, particularly in occupational and physical therapy. It represents therapeutic activities involving dynamic and functional movement, crucial to improving patients’ real-world functional performance. Whether you’re a healthcare provider, medical coder, or therapy clinic owner, understanding the correct use of this code is essential for accurate billing and full reimbursement.
In this comprehensive guide, we’ll break down everything you need to know about the 97530 CPT code, from its definition and billing rules to modifier usage, common code pairings, and practical documentation tips. Let’s dive into the most complete explanation available online.
What Is the 97530 CPT Code?
The American Medical Association (AMA) provides the following description of the 97530 CPT code:
Therapeutic activities involve engaging the patient directly in one-on-one sessions with the clinician, using dynamic exercises aimed at enhancing functional performance. Each session lasts 15 minutes.
This code is used when a healthcare provider conducts goal-directed, functional activities with the patient—such as lifting, pushing, pulling, bending, reaching, or simulating tasks like dressing, grooming, or job-specific functions. These activities often have a cognitive component, like planning or sequencing tasks.
When Should You Use CPT Code 97530?
The 97530 CPT code should be used when therapy involves active participation by the patient in dynamic tasks aimed at improving strength, balance, coordination, range of motion, or mobility.
Examples of valid scenarios for billing this code include:
- Simulated kitchen tasks to improve a patient’s ability to return home safely
- Reaching and bending tasks to restore range of motion after surgery
- Lifting, throwing, or pulling activities to build strength after an injury
- Role-play tasks for daily living activities (ADLs/IADLs)
These tasks should have therapeutic intent, with the provider offering skilled interventions during the activity.
CPT 97530 Is a Timed Code
The 97530 CPT code is billed in increments of 15 minutes, adhering to the 8-minute rule that’s widely recognized by Medicare and other insurance providers.
8-Minute Rule Recap:
- You must provide at least 8 minutes of direct treatment to bill for one unit.
- For multiple time-based services on the same day, you combine the minutes and divide by 15 to determine total units.
| Minutes | Units to Bill |
|---|---|
| 8–22 | 1 unit |
| 23–37 | 2 units |
| 38–52 | 3 units |
Always round down to the nearest full unit unless otherwise directed by the payer.
Proper Documentation for 97530 CPT Code
For compliance and reimbursement, it’s crucial to document the following:
- Specific activity performed
- Therapeutic goal (e.g., increase ROM, improve ADL independence)
- Level of assistance provided
- Clinical reasoning for choosing the activity
- Time spent in direct contact with the patient
Poor documentation can lead to denials or audits, so clarity is key. Use strong action verbs like “instructed,” “guided,” “facilitated,” and “monitored.”
Modifier Use with CPT Code 97530
Using modifiers can make it easier to understand the services provided, especially when several procedures are carried out at once. The most commonly used modifiers with 97530 CPT code include:
Modifier 59 – Distinct Procedural Service
Use when 97530 is performed in a separate and distinct session from another service (like 97140 for manual therapy). It bypasses NCCI edits when supported by documentation.
GO / GP – Provider Type
- GO: Occupational therapy
- GP: Physical therapy
Make sure to use the correct one depending on your provider specialty.
Billing 97530 CPT Code with Other Codes
Therapists often perform more than one service in a single session. Here’s how 97530 CPT code interacts with common therapy codes:
97530 + 97140 (Manual Therapy)
Allowed if distinct and separate. Use Modifier 59 with 97530 and document accordingly.
97530 + 97153 (ABA Therapy)
Not allowed—NCCI edits prohibit billing these codes together, even with a modifier. Must be billed on different days.
97530 + Evaluation Codes (e.g., 97161–97163)
Historically, some insurers like Medicare Part B restricted same-day use, but recent rule changes have lifted these restrictions. You can now bill an evaluation and 97530 together when appropriately documented.
Beware of Multiple Procedure Payment Reductions (MPPR)
Many insurers, especially Medicare and Blue Cross/Blue Shield, apply MPPR rules when multiple therapy codes are billed together. This affects how much is reimbursed for the second and subsequent procedures on the same day.
To maximize reimbursement:
- Space out services across multiple days when clinically appropriate
- Always bill the most complex/time-consuming code first
- Monitor payer-specific rules for percentage reductions
Common Billing Mistakes to Avoid
Avoid these common errors when using the 97530 CPT code:
- Billing when the patient arrives late or leaves early (you must document actual time)
- Using the code for passive treatments (like heat or massage)
- Failing to apply modifier 59 when necessary
- Skipping detailed documentation of functional improvement goals
It’s important to keep in mind that if it’s not recorded, it might as well not have occurred—especially from the perspective of insurers.
Real-Life Examples of Using 97530 CPT Code
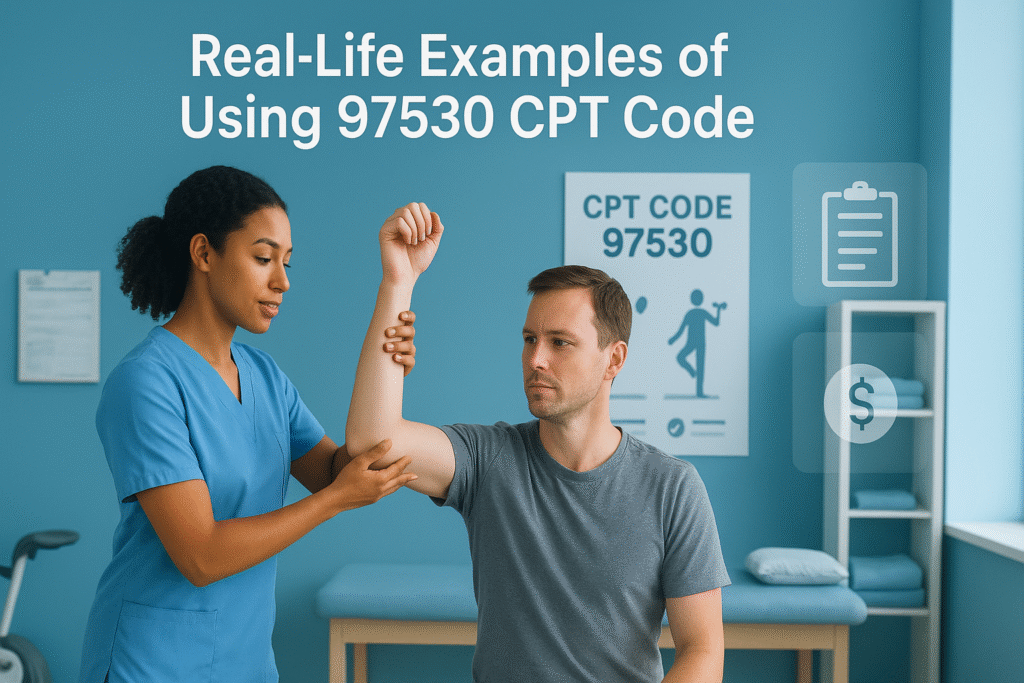
Let’s look at a few realistic scenarios where the 97530 CPT code applies:
Scenario 1
A post-op hip replacement patient is guided through simulated stair climbing, standing-to-sit transfers, and bed mobility exercises to prepare for safe discharge.
Code billed: 97530 x 2 (30 minutes)
Scenario 2
A stroke patient works on reaching and lifting tasks using weighted objects to retrain upper limb function and coordination.
Code billed: 97530 x 1 (15 minutes) + 97110 x 1 (therapeutic exercise)
Insurance Reimbursement Tips for 97530
To ensure smooth reimbursement:
- Confirm that the 97530 CPT code is covered by the payer
- Use clear documentation of goals, activities, and time
- Apply appropriate modifiers (especially Modifier 59)
- Stay updated on payer-specific rules for bundling, edits, and reductions
Consider using billing software or outsourced RCM services if your clinic struggles with denials or payer policy tracking.
Conclusion
The 97530 CPT code is an essential billing code for physical and occupational therapists, representing skilled, goal-driven therapeutic activities that help patients regain functional independence. Using incorrect procedures or inadequate documentation may result in payment denials or trigger audits.
To bill 97530 CPT code properly:
- Ensure skilled, dynamic activity is performed
- Accurately track time and follow the 8-minute rule
- Use correct modifiers like 59 and GO/GP
- Document thoroughly and clearly
- Understand payer-specific bundling and MPPR rules
When used correctly, this code not only supports accurate billing but also reflects the real value therapists provide in patient recovery.
Frequently Asked Questions (FAQs)
What is the 97530 CPT code used for?
The 97530 CPT code is used to bill for therapeutic activities involving dynamic, functional movement aimed at improving strength, coordination, or daily living skills.
Is CPT 97530 a timed code?
Yes, it’s billed in 15-minute units and follows the 8-minute rule for time-based coding.
Can you bill 97530 with 97140?
Yes, but only in the event that the services are unique and separate. You must apply Modifier 59 to 97530 and clearly document the difference.
Can you bill 97530 and 97153 together?
No. These codes are subject to NCCI edits and cannot be billed together, even with a modifier.
Does CPT code 97530 require a modifier?
Yes, in many cases. Use Modifier 59 when needed and GO/GP modifiers to indicate the type of therapy provider.
In a single session, how many units may I bill for 97530?
The quantity of time spent with the patient personally is what matters. For example, two units are equal to thirty minutes.
Does 97530 fall under MPPR rules?
Yes. If you bill multiple therapy codes in one session, MPPR may reduce reimbursement for secondary procedures.
