Introduction
The 80053 code for CPT is like a lab test thing, lots of people see on bills or papers from insurance. But most folks don’t really know what it is, when doctors use it, or how it changes the money part. In this article, I will explain the 80053 CPT code in simple, clear terms. You will learn its definition, uses, billing tips, insurance issues, and also some real‑world examples. After all this, you will know more about what 80053 CPT code mean when you see it on paper or bill.
What is 80053 CPT code?
It’s a code from the CPT system (that’s like how doctors and labs name stuff thSystem. system. It is used to identify a specific laboratory panel in medical billing and coding. When a doctor orders a broad “comprehensive metabolic panel,” labs often use the 80053 CPT code to capture that detail in bills.
In other words, the 80053 CPT code is a numeric label that tells insurers, hospitals, and labs: “This is that lab test package with multiple individual tests inside.” The CPT system is there to make naming stuff the same, so doctors, insurance, and people all know what got done.
Components of 80053 CPT Code
Inside the 80053 CPT code panel, multiple tests are grouped. These usually include measurements like:
- Electrolytes: potash, sodium, and chloride
- Kidney test: creatinin, BUN
- Liver thing: ALT, AST
- Sugar test (glucose)
- Total protein and albumin
- Bilirubin
- And others
Since 80053 Chascode got a lot of tests incosts it costs more than just one small test. Bushows show more info about how the main organs in he body are doing.
When do they use the 8005A doctor?

A doctor or healthmaymayer may ask for this test when someone feels tired, weak, has stomach hurt, or if they checking on a long-time illness. Some the the use 80053 CPT code as part of routine health exams when comprehensive checks are needed.
Here are typical situations:
- Yearly doctor visits: To see normal stuff for body organs.
- Watching long-term sickness: Like for people with a sugar problem (diabetes), liver trouble, or other problems.
- Checking strange feelings: If somefeelsf,, eel sick, like throwing up, swelling, or has had weird test results before.
- Before surgery: Sometimes doctors ask for this big test before doing an operation.
So, whenever many body systems must be checked at onthe the ce, the 80053 CPT code is one of the go‑to options.
Billing and Coding Tips for 80053 CPT Code
Since 80053 CPT code is a bundled panel, billing must be accurate. Here are some tips:
- Use it only when the full panel is done. If only a few of those tests are done, you should bill individual codes, not the 80053 CPT code.
- Avoid duplication. If parts of that panel were already done in another test order, you should not double‑bill.
- Modifier usage. If a portion is done separately or by another lab, sometimes modifiers may be needed.
- Insurance awareness. Some insurers may prefer you to break out smaller tests instead of using a full panel, the tthe80053 CPT code, depending on policy.
- Document well. Always keep a record of all the CPTT codes that were completed, or note why some parts were omitted.
By following these, you reduce the chance of claim denials when using the 80053 CPT code.
Insurance Coverage and Challenges With 80053 CPT Code
Though the 80053 CPT code is standard, many insurance plans have rules:
- Preauthorization requirements. Some insurers may want you to justify why this broad panel is needed before approving payment.
- Coverage limits. They may only cover certain parts or refuse bundle codes if they consider them “unnecessary.”
- Patient cost share. Even if covered, patients may pay copayments, coinsurance, or deductible amounts for tests under the 80053 CPT code.
- Denied claims. If coding errors or missing justification occur, claims with the 80053 CPT code could be denied.
- In‑network vs out‑of‑network. Tests done outside the insurer’s preferred labs may lead to partial or no coverage for the 053 CPT code.
Therefore, before ordering or billing the 80053 CPT code, chthe eck patient’s insurance plan and rules.
Doing the 80053 test – here’s kinda how it can go:
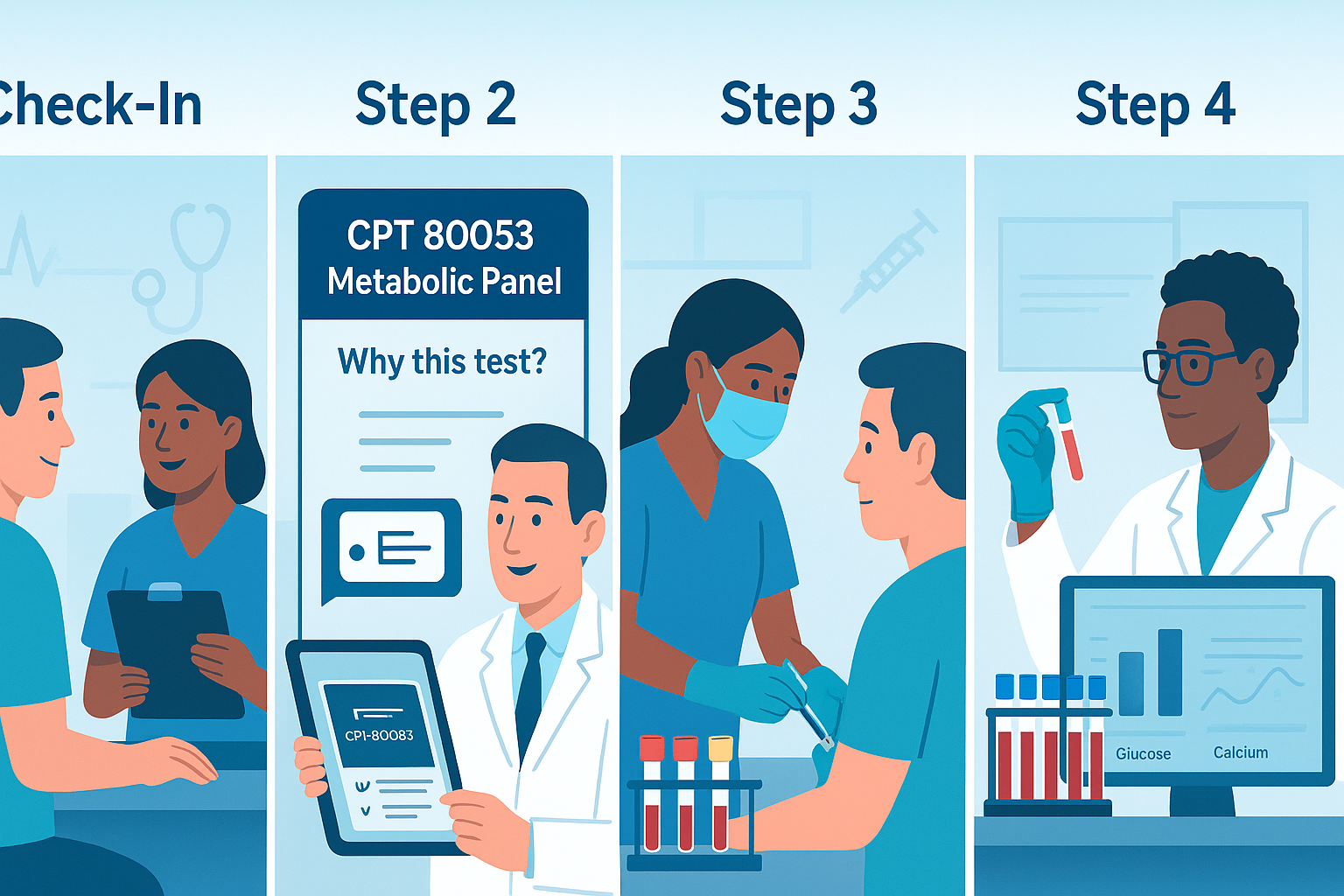
- Doctor thinking: The doctor sees the patient has some swelling, is really tired, and had a liver test come out not right before.
- Order placed: Doctor orders “comprehensive metabolic panel (CPT 80053).”
- Lab collects samples: Blood is drawn, and samples are sent to the lab.
- Lab work: The lab does all the tests that come with the 80053 code.
- Making the report: They put all the test numbers together, like sugar (glucose), creatinine, ALT, and others.
- Billing coding: Lab or hospital codes as 80053 CPT code (plus any modifiers if applicable).
- Claim submission: Sent to insurer.
- Insurance review: The Insucheckssthe if the panel is covered, whether justification is present.
- Payment or denial: Either insurer pays, pays partially, or denies.
- Patient bill: Patient sees any remaining balance, which may include a portion of the 80053 CPT code cost.
This workflow is typical when the 80053 CPT code is used.
Pros and Cons of Using 80053 CPT Code
Pros
- Covers a lot: You get lots of test results from just one order.
- Simple process: Just one order, one blood draw, and done in one go.
- Good for unclear stuff: Helps when the doctor is not sure what’s wrong.
- Standardization: Being a standard code, it’s widely accepted (if documented properly).
Cons
- Cost: More expensive than individual tests.
- Insurance risk: A greater chance of denial if the justification is weak.
- Overtesting concern: Some might argue that not all components were ne, ded—leading to waste.
- Redundancy: Some tests might duplicate others, causing overlapping billing issues.
Because of those, providers sometimes hesitate to use the 80053 code unless needed.
Tips for Patients When They See 80053 CPT Code
If you are a patient and your bill or insurance explanation shows the 80053 CPT code, here are things you can do:
- Ask your doctor what each test was for. Request an explanation of why the full panel.
- Get itemization. Ask the lab or provider to show which tests were included under the 80053 CPT code.
- Check insurance plan. Look to see whether your plan covers that panel or whether it requires justification.
- Ask about cheaper alternatives. It might be possible to run only certain tests rather than the full panel.
- Appeal denials. If the insurer denies the claim, you can often appeal with documentation from your physician justifythe ing the need for the 80053 CPT code.
By doing so, you may reduce your costs or avoid surprises when the 80053 CPT code appears.
Good ways for doctors to use the 80053 CPT code
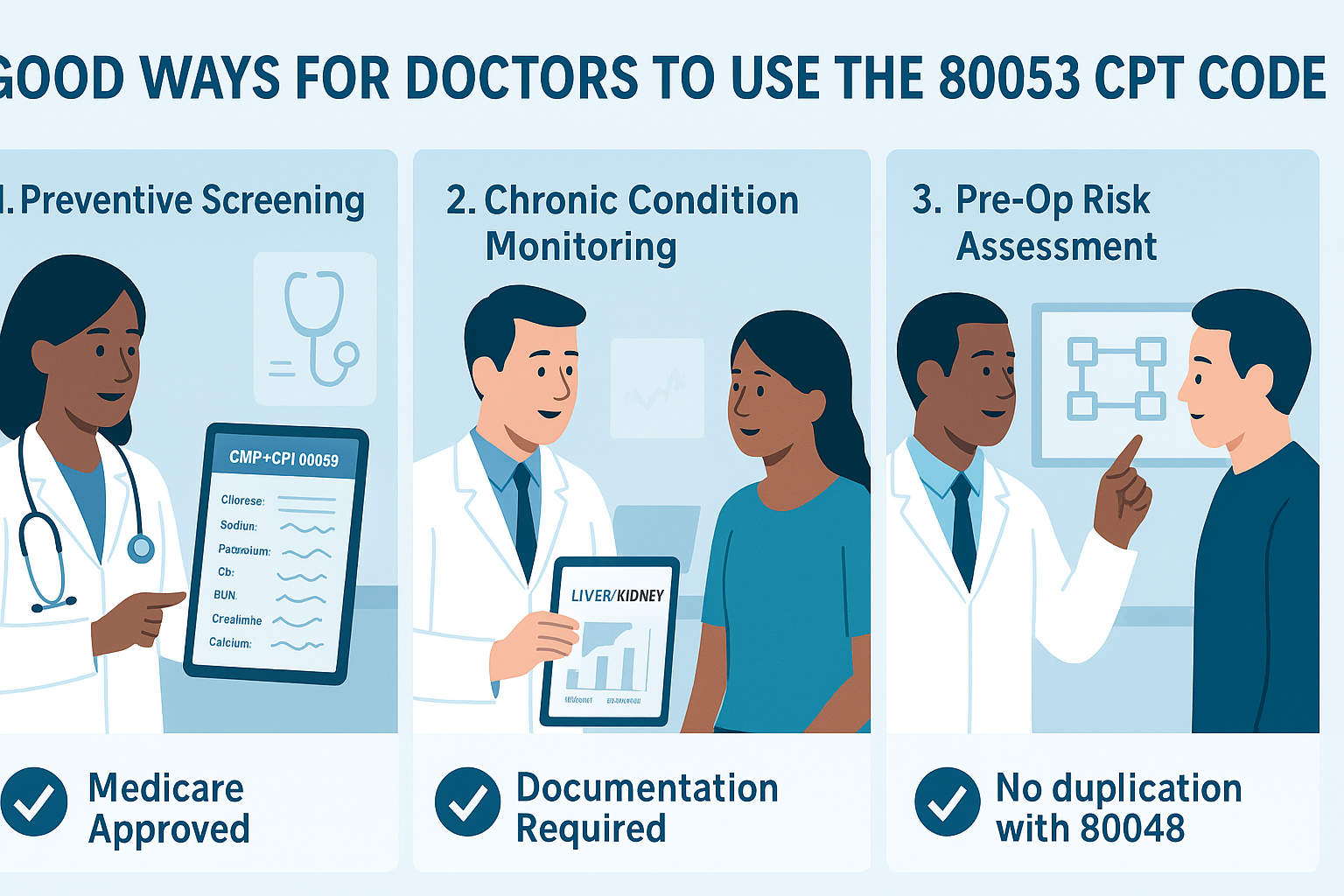
To use the 80053 code correctly and avoid billing trouble, doctors should:
- Check with the patient’s insurance first if they pay for 80053.
- Keep notes in the patient’s file about why they ask for the full test.
- Don’t order tests that repeat stuff already in 80053.
- Use correct modifiers if part of the panel is done elsewhere.
- Monitor denial patterns — if certain insurers often reject the 80053 CPT code, consider alternate strategies.
- Train billing staff about the nuances of the 80053 CPT code so errors are minimized.
By following these, you reduce stress on both provider and patient for the 80053 CPT code billing.
Real‑World Example: Cost and Coverage
Here is one example to show how 80053 CPT code work in real life:
A clinic order 80053 test for patient who have high blood pressure and strange lab results.
The lab charges $80 for the full panel.
The patient’s insurance plan covers “comprehensive metabolic panels” but only if justified.
Insurance approves $ 60, patient’s coinsurance is 20%. So insurance pays $60, patient pays $14 (20% of $70 allowed amount) plus any deductible remainder.
the
If insurer denies it due to a lack of justification insured may receive the full $80 bill unless the appeal succeeds.
This shows how the cost and payment of the 80053 CPT depend heavily on policy details.
Summary and Conclusion
The 80053 CPT is a widely used lab panel code that bundles many important tests into one order. It helps doctors assess multiple organ systems at once. But because it is broad, proper documentation, smart billing, and insurance knowledge are essential.
If used well, the 80053 CPT can benefit both provider and patient by giving comprehensive data efficiently. If used carelessly, however, it can lead to denials, wasted tests, or high patient bills. As a patient or provider, always check the justification, insurer rules, and possibility of scaling down to individual tests if needed.
Whenever you see the 80053 CPT code in a report or bill, you can now ask informed questions: Why was it ordered? Which tests did it include? Was it all done? Was insurance coverage appropriate?
